The two most common conditions associated with the brain in myelomeningocele are hydrocephalus and arnold chairi II malformation.
Hydrocephalus
The brain is surrounded by a clear, saltwater-like liquid called cerebrospinal fluid (CSF). CSF protects and nourishes the brain. It flows in a circuit through the brain cavities (ventricles) and over the surface of the brain and spinal cord. It is continuously reabsorbed by the body. Hydrocephalus occurs when there is an obstruction to the flow of CSF, causing fluid to build up within the cavities of the brain. This fluid build-up can cause pressure on the brain tissues and bones of the skull.
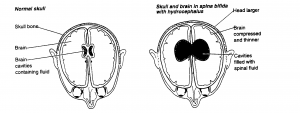
Most children (about 85%) with myelomeningocele will have hydrocephalus. Often the collection of fluid does not become severe until after the myelomeningocele has been surgically closed so it may not become evident until the first few days or weeks after your child’s birth.
How is Hydrocephalus Detected and Monitored?
In an infant, the plates of the skull are not yet fused together. The plates are therefore able to shift and accommodate the excess cerebrospinal fluid and thus lessen the impact on the brain. As fluid accumulates, a child’s head circumference increases in size (distance around your child’s head). Hydrocephalus is detected and monitored through regular measurement of your child’s head circumference. Other symptoms such as sleepiness, poor feeding, vomiting, or irritability may also be present. Hydrocephalus can also be detected through scanning of the head. (Ultrasound, CT scan and MRI).
How is Hydrocephalus Treated?
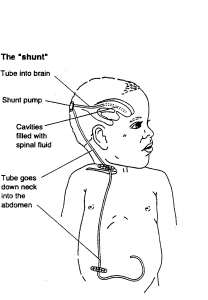
Hydrocephalus is usually treated by insertion of a shunt – this is a device that drains, using a one-way valve, excess CSF from the brain to another part of the body, usually the abdominal cavity (stomach). Draining the excess fluid relieves any symptoms of hydrocephalus that are present. Your neurosurgeon will decide if and when your child needs a shunt.
This commonly occurs following surgical closure of the myelomeningocele, but sometimes it is done before the closure and sometimes on the same day. If a shunt is required, it will always be necessary. A shunt is for life, although a child may need their shunt replaced a few times in their lifetime. Shunts generally work well but problems can arise. Shunts can become infected, blocked or, they can twist and break. The tube from the brain to the abdomen can become too short as the child grows. Surgery may be necessary to remove or replace the shunt or lengthen it as needed.
About 40% of shunts fail in the first year for a variety of reasons. If this happens, CSF will begin to accumulate again. Problems may occur suddenly or develop gradually.
Signs and symptoms will vary with age and from individual to individual. You should seek prompt medical attention if you observe your child experiencing any of the following symptoms:
- Full or bulging fontanelle (soft spot)
- Seizures
- Enlarged head size
- Headache
- Swelling or redness along the shunt tract
- Fever
- Irritability
- Vomiting
- Drowsiness
- Loss of previous abilities
- Change in appetite
- Prominent veins on scalp
It is very important for parents and health care workers to be aware of the signs of a shunt problem and to take the child to the doctor or local hospital if they are concerned.
If your child has mild hydrocephalus, they may not require a shunt. They will need to be checked regularly for signs of evolving hydrocephalus. You should also be aware of these signs as you will need to seek medical attention if you are concerned that your child’s hydrocephalus is progressing.
Chiari II malformation (also known as Arnold- Chiari malformation)
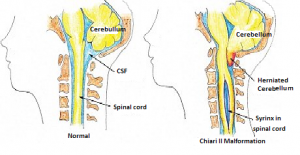
Chiari II malformation (pronounced Key – ar- ee) is a congenital malformation of the spine and posterior fossa which is commonly seen in children with myelomeningocele. Chiari II malformation is made up of a number of features including:
- Small posterior fossa (part of skull at the back of head which contains the cerebellum)
- Cerebellar herniation (brain tissue extending into the spinal canal)
- Cerebellar and brainstem deformity and descent
- Midbrain abnormalities (tectal beaking)
- Hydrocephalus
- Cortical abnormalities (disorganized brain development)
- Grey matter heterotopia (disorganized brain development)The resulting brain abnormalities can contribute to a child with spina bifidas overall disability. In general there is a higher incidence of intellectual and behavioral problems in this population and a higher risk of epilepsy also
After hydrocephalus, cerebellar and brainstem abnormalities are the next most important part of the Chiari 2 malformation. It is found in almost all children born with Myelomeningocele.
How can Chiari II malformation affect your baby?
Chiari II malformation mainly involves the lower brainstem and lower most portion of the cerebellum, but the layout of the whole brain is also affected. The brainstem contains many of the nerves which control the heart, breathing, blood pressure and help control swallowing, sneezing and coughing. The cerebellum controls the posture and coordination of muscle action to produce precise, coordinated movements.
Your child will have had an MRI to examine the structure of their brain and spinal cord.
When the Chiari II malformation is present, the skull space at the base of the brain is smaller and therefore the brainstem is elongated and displaced downwards into the opening of the base of the skull and top of the spinal canal. The brainstem, cranial nerves and the lower portion of the cerebellum may be stretched or compressed and any of the functions controlled by these areas may be affected.
Chiari II and Hydrocephalus
The malformation might also block the flow of cerebrospinal fluid causing hydrocephalus. Most children with Chiari II malformation have no obvious symptoms and therefore need no treatment .
Some children however do develop symptoms (about 5% in our population). You should contact your doctor promptly if your child develops any of these symptoms. Symptoms may be related to faulty shunt function, poorly controlled hydrocephalus or brainstem compression.
Symptoms of Arnold Chiari malformation at different developmental stages
| Infancy | Childhood |
| Stridor (noisy breathing) | Arm tightness or weakness |
| Weak or absent cry | Stiff neck |
| Arching of their neck backwards | Feeding or breathing difficulties |
| Breathing difficulties | Increasing problems with hand eye coordination |
| Feeding or swallowing difficulties | |
| Hypersensitivity to objects in their mouth |
Please note: as your child develops, the symptoms may present differently.